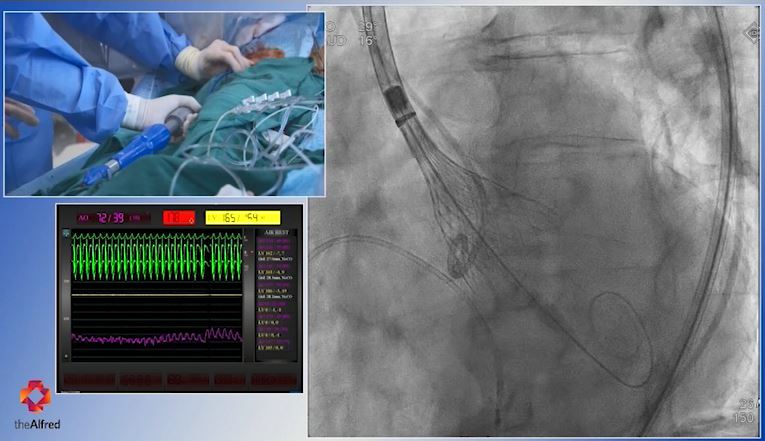
Watch highlights of a Transcatheter Aortic Valve Implantation performed recently by cardiologists A/Prof Tony Walton, Prof Stephen Duffy and A/Prof Dion Stub at The Alfred. The procedure involves passing a catheter (a small tube) through an artery from the groin up into the heart. This was broadcast live from our cath lab to a major cardiology conference.
Alfred Health Life:
Heart
“Our cardiac program is unique. We can take a clinical problem to the research lab, figure out a new treatment or test, and bring it back to the bedside. There are very few centres nationally and internationally able to do this.”
Prof David Kaye, Director of Cardiology
Valve replacement without surgery
More patients suffering from a common heart condition may soon have the option of avoiding surgery as new evidence emerges about the best way to treat a narrowing of the aortic valve.
The Alfred was the lead Australian hospital in a global trial of patients looking at whether a minimally invasive technique to replace the heart valve – without need for open heart surgery – was suitable for more patients suffering aortic stenosis.
Director of The Alfred’s cardiac laboratories and interventional cardiologist, A/Prof Tony Walton said the procedure known as Transcatheter Aortic Valve Implantation (TAVI) was a revolution in treatment.
“Aortic stenosis causes an abnormal narrowing of the aortic valve, which means the heart can no longer pump blood efficiently,” A/Prof Walton said.
“Using TAVI, a biological tissue valve is inserted on a catheter that is guided to the heart through a major artery, often the femoral artery starting at the groin.
“We thought TAVI would be about the same in terms of outcomes compared with surgery, but TAVI turned out to be superior – causing less injury to the body, a faster recovery time and shorter stay in hospital.
While study data revealed the cath lab-based procedure carried a reduced risk of causing stroke or death than surgery, instances where a pacemaker was needed were greater.
“Traditionally, only high-risk patients unsuitable for open heart surgery were candidates for TAVI but we now consider all patients in their late 60s and 70s.”
The international study was published in the New England Journal of Medicine DOI:10.1056/NEJMoa1816885

Mauro survives with ECMO collaboration
Geelong-based businessman Mauro was fit and hardworking, and never imagined he’d one day be clinging to life in the intensive care unit at The Alfred.
“I always considered myself bulletproof and nothing ever stopped me,” said the 60-year-old father of four.
After suffering a heart attack, Mauro’s doctors said he needed quadruple bypass surgery and a new heart valve. Still, Mauro thought he’d be back at work in no time.
“I remember being wheeled into the operating theatre in Geelong, then a lot of freaky dreams, then I woke up in the intensive care unit (ICU) at The Alfred,” said Mauro.
After the surgery, Mauro experienced a rare condition called cardiogenic shock. His heart wasn’t pumping enough blood and he needed life support. The team at Geelong Hospital connected him to an extracorporeal membrane oxygenation (ECMO) machine and contacted The Alfred.
ICU nurse and ECMO specialist, Jayne Sheldrake, received the call requesting assistance.
“It was clear he needed in-depth cardiac support, more investigations, and time on ECMO for his body to recover,” said Jayne.
Jayne travelled to Geelong with intensive care specialist A/Prof David Pilcher to retrieve Mauro. And, once back at The Alfred, critical care nurse Malcolm Stewart remained at Mauro’s side hour-after-hour.
“It’s important we communicate with our patients, and that’s what I did with Mauro. I let him know what was going on, that he was in a safe place and was getting better," said Malcolm. “ECMO gave him a second chance at life.”
After more than two weeks on the specialised life support, under the watch of an internationally regarded team, Mauro’s heart began to recover. It wasn’t long before he was back home and building strength through rehabilitation.
Mauro recently celebrated his 60th birthday and returned to The Alfred’s ICU to meet with some of his care team.
“It’s rewarding and emotional to see Malcolm and the other doctors and nurses. I will never forget them,” said Mauro, who’s now dreaming of travel and relaxation.

Women's heart clinic a Victorian first
Heart disease is the number one killer of Australian women. Despite this, much of what we know about heart disease comes from studies that have been conducted on male hearts. Recognising that women need specialised care, The Alfred established Victoria’s only Women’s Heart Clinic earlier this year.
Run by cardiologist Monique Watts, the clinic has provided specialised care and education to dozens of women about female-specific heart problems.
“Women are more likely to suffer from different types of heart attacks to men, and they are not always best treated by the conventional therapy we use,” Dr Watts said.
“We’re becoming more aware that heart disease affecting women is often very different to the type of heart disease affecting men, and women’s heart clinics are able to facilitate much-needed gender specific research.”
Dr Watts said one patient in particular has stood out to her this year.
“This patient had been suffering chest pain for 12 years and conventional care had failed her - she had seen many different doctors with no improvement,” she said.
“The patient was suffering from a condition called coronary vasospasm where the coronary artery constricts in an unpredictable fashion and restricts blood flow to the heart muscle - causing chest pain.
"After specific testing and appropriate treatment, she is pain free for the first time in 12 years. This is extremely rewarding.”
Women experience unique risk factors, like complications in pregnancy including diabetes or hypertension – which leaves them more likely to develop heart disease at a young age, Dr Watts said. She recommended all women talk to their doctors about their heart health, know the warning signs of heart attack and ensure any risk factors are being addressed.

Miniature heart pump a life saver
Alfred cardiologists have used a miniature heart pump to keep a Melbourne-man alive during a high-risk stent procedure.
Director of the Catheter Laboratory, A/Prof Tony Walton, said his patient’s heart had become so weak due to blocked arteries that the team was concerned he wouldn’t make it through.
“We anticipated a long procedure due to the calcification in Stephen’s (patient) arteries – it acts like concrete and makes it harder to work – so the risk to him was very high,” Dr Walton said.
To support Stephen’s heart and blood pressure during the stenting procedure, doctors first inserted the powerful pump, called Impella, through his right femoral artery and placed it inside his left ventricle chamber.
“The pump delivers most of what a heart needs to do. Even if the heart stopped completely there would still be enough circulation to keep going while we rectified the problem.”
“The Impella sucks blood out of the chamber at 3.5 litres per minute (a normal heart can deliver five litres per minute) and delivers it into the aorta.”
With Stephen’s heart supported by the Impella, Dr Walton and the team were able to work on his arteries, accessing the heart through the right radial artery. They then inserted the stents, which hold open the narrowed arteries and restore blood flow to the heart.
“This is a Victorian first that will allow us to give the sickest of the sick a better chance during complex procedures or during a heart attack," said Dr Walton.

Alcohol-induced heart attack the unlikely answer
A unique procedure, which involves the use of alcohol to induce a controlled heart attack is restoring quality of life for a small number of patients.
Interventional cardiologist A/Prof Will Chan is one of few Australian doctors using the technique, known as alcohol septal ablation, as a treatment option for patients where open heart surgery is not recommended.
“Patients with hypertrophic obstructive cardiomyopathy have a thickened heart muscle, which will increasingly obstruct the blood flow. If left untreated, the condition can eventually cause significant breathlessness, chest pains, dizziness, and sometimes death,” A/Prof Chan said.
“While surgeons can cutback the thickened muscle, they first need to stop the heart. Patients who have previously had open heart surgery, or who are older or frail, are often poor candidates for such an invasive procedure.”
Prof Chan said alcohol septal ablation may be the answer in these cases, and can help normalise heart function.
“The procedure involves the injection of pure alcohol directly into the overgrown heart muscle to create a localised chemically-induced heart attack,” A/Prof Chan said.
“The alcohol is toxic to the heart cells and causes them to die. As the cells shrink, the overgrown muscle reduces in size, and blood flow is improved.”
The Alfred is one of the only Victorian hospitals that offers this treatment option.